National Lung Cancer Screening Program
- About
- Eligibility
- MBS items and billing
- National Cancer Screening Register
Program guidelines and summary
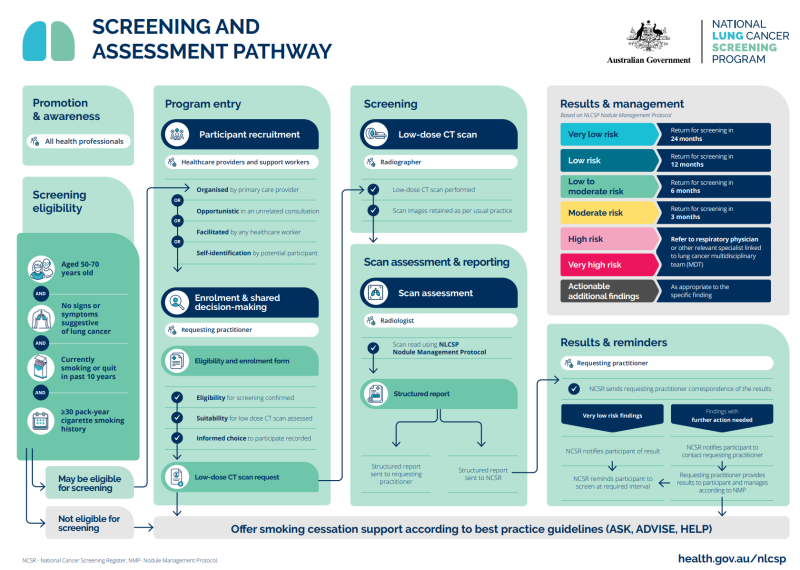
The National Lung Cancer Screening Program (NLCSP) is a targeted screening program using low-dose computed tomography (low-dose CT) scans to look for lung cancer in high-risk people without any signs or symptoms suggestive of lung cancer.
Refer to the NLCSP Program Guidelines for information on:
-
Patient eligibility
-
Screening and assessment pathway
-
Reporting scan results
-
Nodule management protocol
-
Actionable additional findings
Visit HealthPathways for local referral pathways and other information.
 |
 |
To be eligible for NLCSP patients must be:
-
Aged between 50 and 70 years
-
Asymptomatic and
-
have a history of at least 30 pack-years of cigarette smoking and are still smoking, or
-
have a history of at least 30 pack-years of cigarette smoking and quit in the past 10 years.
Identifying patients who may be eligible
As this is a targeted screening program the NCSR will not be sending invitations to potentially eligible patients. It is recommended that patients’ smoking histories be routinely updated in clinical software to make it easier to identify patients who may be eligible to join the program.
Plan and implement the below three steps as a quality improvement activity, which can also be undertaken as part of the QI PIP.
-
Patients 15+ who do not have their smoking status recorded can be identified using the PenCAT tool, and a list created.
-
Refer to the SPDS manual for Best Practice or Medical Director provided by COORDINARE. For assistance contact your local COORDINARE Health Coordination Consultant.
-
Set up prompts in clinical software for those patients who may be eligible to facilitate opportunistic discussions.
Two new Medicare Benefit Schedule (MBS) items will be created to provide low-dose computed tomography (LDCT) scans under the NLCSP.
-
The screening LDCT scan done by the participant every 2 years
-
The interval LDCT scans for any follow-up needed during the 2-yearly screening period (as required following results of the screening LDCT test).
These will be mandatory bulk billing items for radiology and will have mandatory reporting requirements. Refer to MBS website from 1 July.
Bulk-billing of GP consultations to refer for screening and manage results is not mandatory.
The NLCSP will be added to the National Cancer Screening Register alongside the National Cervical Screening and National Bowel Screening Programs.
The National Cancer Screening Register (NCSR) will be integral to the operation of the NLCSP by providing participant reminders and giving healthcare providers access to patient records and ability to submit reports.
To streamline access, GPs and providers can integrate their clinical software with the NCSR. For more information click on the prepare tile.
National Lung Cancer Screening Program: Get your practice ready
- Get your practice ready
- Connect directly to the NCSR
- Identify patients who may be eligible
- Local HealthPathways
Get your practice ready for the NLCSP
The National Cancer Screening Register (NCSR) will be integral to the operation of the NLCSP. By integrating their clinical software with the National Cancer Screening Register GPs, nurses and Aboriginal health practitioners will have real-time access to a patient’s record without a separate NCSR login, and can access screening histories and reports, update details and submit forms.
Step-by-step instructions for integrating BP, MD and Communicare can be found here or in the Primary Care Onboarding Kit.
For assistance call the NCSR helpline 1800 627 701 or request a callback NCSR: Registration Help.
You can also contact COORDINARE's digital health team digitalhealth@coordinare.org.au or your local COORDINARE Health Coordination Consultant.
As this is a targeted screening program the NCSR will not be sending invitations to potentially eligible patients. It is recommended that patients’ smoking histories be routinely updated in clinical software to make it easier to identify patients who may be eligible to join the program.
Plan and implement the below three steps as a quality improvement activity, which can also be undertaken as part of the QI PIP.
-
Patients 15+ who do not have their smoking status recorded can be identified using the PenCAT tool, and a list created.
-
Refer to the SPDS manual for Best Practice or Medical Director provided by COORDINARE. For assistance contact your local COORDINARE Health Coordination Consultant.
-
Set up prompts in clinical software for those patients who may be eligible to facilitate opportunistic discussions.
Access the Lung Cancer Screening Program Calculator here.
Proxy Pack Year Calculator for Aboriginal and Torres Strait Islander Patients here.
National Lung Cancer Screening Program: key resources and information for:
- GPs and other healthcare providers
- Patients
- Rural communities
Webinars
National Lung Cancer Screening Program - South Eastern NSW
Illawarra Shoalhaven - NLCSP a practical approach Illawarra Shoalhaven
Resources
- National Lung Cancer Screening Program – Healthcare provider toolkit | Australian Government Department of Health, Disability and Ageing
-
DOHDA National Lung Cancer Screening program factsheets and guides
- General Practitioner Resource Guide
-
DOHDA National Lung Cancer Screening program guidelines - you access a summary of these guidelines here.
Education
-
The Lung Foundation offers six free CPD accredited, eLearning modules on the National Lung Cancer Screening Program. Learn more here.
-
The Lung Learning Hub provides tailored education and training to optimise patient care. Assess your skills using the Lung Learning Framework - Australia’s best-practice standard for lung care - and access other quality evidence-based training. Learn more here.
-
Quit Centre online training modules and events for GPs, Nurses, Aboriginal Health Practitioners and other health professionals. Learn more here.
DOHDA community resources:
- Fact sheets and guides
- What is the NLCSP factsheet
- Frequently asked questions from community members
Aboriginal and Torres Strait Islander peoples resources:
Support and resources for patients:
Heart of Australia has partnered with the Australian Government to co-deliver the new National Lung Cancer Screening Program (program) by providing mobile lung cancer screening services to rural and remote communities nationwide.
The program will roll out from July 2025 and will enable earlier detection of lung cancer in Australia. Learn more here.